
Wound care certification is crucial for healthcare professionals, enhancing patient outcomes and professional competence. A comprehensive study guide provides essential knowledge, preparing candidates for certification exams and practical application.
1.1 Importance of Wound Care Certification
Wound care certification is vital for healthcare professionals, as it ensures standardized, evidence-based practices, improving patient outcomes. Certification validates expertise, enhances credibility, and demonstrates commitment to quality care. It also reduces complications, promotes efficient healing, and minimizes healthcare costs. Additionally, certified professionals contribute to better infection control and overall wound management, making it a cornerstone of modern healthcare.
1.2 Overview of the Certification Process
The certification process involves meeting eligibility criteria, such as clinical experience and education, followed by a comprehensive exam. Candidates prepare using study guides covering wound assessment, healing stages, and infection control. The exam tests knowledge and practical skills, ensuring expertise in evidence-based wound care. Certification is maintained through continuing education, reflecting industry advancements and best practices.
1.3 Benefits of Becoming Certified
Certification enhances professional credibility and expertise in wound care, leading to improved patient outcomes. It demonstrates a commitment to evidence-based practices and fosters career advancement opportunities. Certified professionals often experience increased confidence in their abilities, contributing to better patient care. Additionally, certification can open doors to specialized roles and leadership positions in healthcare settings.

Key Topics Covered in the Study Guide
The study guide covers wound assessment, classification, and healing physiology. It also addresses infection control, nutritional considerations, and advanced wound care products, ensuring comprehensive preparation.
2.1 Wound Assessment and Classification
Wound assessment and classification are foundational skills for effective wound care. The study guide details methods for evaluating wound depth, severity, and tissue type. Classification systems, such as acute vs. chronic wounds, and grading by depth (e.g., Stage 1 to 4 pressure ulcers) are explored. Understanding these concepts aids in developing targeted treatment plans and improving patient outcomes significantly.
2.2 Physiology of Wound Healing
The physiology of wound healing involves a complex, dynamic process with four main stages: hemostasis, inflammation, proliferation, and remodeling. The study guide explores cellular components and tissue repair mechanisms, emphasizing the role of oxygenation, nutrition, and growth factors. Understanding these biological processes is crucial for developing evidence-based treatment strategies and optimizing patient recovery outcomes in wound care settings.
2.3 Infection Control and Management
Infection control is critical in wound care, preventing complications and promoting healing. The study guide covers identifying infection signs, antibiotic use, and resistance. It emphasizes proper debridement techniques and sterilization methods to manage bacterial loads, ensuring aseptic environments. Effective infection management strategies are essential for reducing risks and improving patient outcomes in wound care settings.
2.4 Nutritional Considerations for Wound Healing
Nutrition plays a vital role in wound healing, with specific dietary elements aiding recovery. The study guide highlights the importance of proteins, vitamins, and minerals like zinc and vitamin C. Proper hydration and personalized dietary plans are emphasized, addressing how malnutrition can impede healing. These insights help healthcare providers optimize patient care and accelerate wound recovery through tailored nutritional strategies.
Wound Types and Classification
Wounds are classified as acute or chronic, based on healing time, and by depth, severity, and cause, influencing treatment approaches and patient care strategies effectively.
3.1 Acute vs. Chronic Wounds
Acute wounds heal within 6-8 weeks, following a predictable recovery timeline, while chronic wounds persist beyond 8 weeks, often due to underlying conditions like diabetes or poor circulation. Acute wounds, such as cuts or burns, typically progress through healing stages without complications. Chronic wounds, like diabetic ulcers, require specialized care and may stem from prolonged inflammation or infection. Understanding these differences is crucial for effective management.
3.2 Classification by Depth and Severity
Wounds are classified by depth and severity to guide treatment. Superficial wounds affect only the outer skin layers, while deeper wounds penetrate underlying tissues and organs. Classification systems help standardize care, ensuring appropriate interventions. Accurate assessment of depth and severity is critical for developing effective treatment plans and improving patient outcomes in wound management.
3.3 Common Causes of Wounds
Wounds can result from trauma, infections, burns, pressure, or diabetic complications. Understanding the cause is key to effective management. Traumatic wounds stem from accidents, while pressure ulcers develop from prolonged immobility. Infections and burns require specialized care. Accurate classification by cause, depth, and severity ensures tailored treatment plans, improving patient outcomes and recovery rates in wound care settings.

Wound Healing Stages
Wound healing occurs in four stages: inflammation, proliferation, remodeling, and cleaning. Each stage is crucial for restoring tissue integrity and achieving optimal recovery from injury or surgery.
4.1 Inflammation Phase
The inflammation phase is the body’s initial response to injury, characterized by bleeding, redness, and swelling. It involves the activation of immune cells, release of chemical mediators, and the formation of granulation tissue. This phase is vital for preventing infection and preparing the wound for the next healing stages. Proper wound assessment and care during this phase are essential for promoting timely recovery and minimizing complications.
4.2 Proliferation Phase
The proliferation phase involves the formation of granulation tissue, epithelialization, and collagen synthesis. This stage is crucial for wound closure and strength. The body rebuilds tissue, and a moist environment promotes healing. Proper wound care, including dressings and topical treatments, supports this phase, ensuring the wound progresses toward full recovery and minimizing the risk of complications.
4.3 Remodeling Phase
The remodeling phase is the final stage of wound healing, lasting up to two years. During this phase, the newly formed collagen remodels, strengthening the tissue. The wound closes, and the scar tissue becomes more durable. Proper care ensures the tissue regains maximum strength, reducing the risk of future injury. This phase is vital for achieving long-term wound integrity and patient recovery.
Infection Management
Infection management is critical in wound care, involving early detection of signs like redness, swelling, and purulent discharge. Proper antimicrobial use and debridement techniques prevent complications and promote healing.
5.1 Identifying Signs of Infection
Identifying infection signs is vital for effective wound management. Common indicators include increased redness, swelling, warmth, and purulent discharge. Monitoring for foul odor, fever, or prolonged healing can signal infection. Early detection allows timely intervention, preventing severe complications and promoting faster recovery.
5.2 Antibiotic Use and Resistance
Antibiotic use in wound care must be judicious to combat resistance. Overuse can lead to resistant bacteria, complicating treatment. Guidelines recommend reserving antibiotics for confirmed infections and selecting based on culture results. Proper stewardship is key to maintaining their effectiveness and reducing resistance rates in clinical settings.
5.3 Debridement Techniques
Debridement involves removing dead tissue to promote wound healing. Techniques include surgical, mechanical, enzymatic, and autolytic methods. Surgical debridement is precise, often requiring skilled professionals. Mechanical uses dressings to physically remove debris. Enzymatic employs enzymes to break down dead tissue without harming healthy cells. Autolytic debridement uses dressings like hydrogels or films to enhance the body’s natural processes. Proper technique selection is crucial for effective wound management.
Dressings and Topical Treatments
Dressings protect wounds, promote healing, and manage drainage. Topical treatments enhance recovery by addressing specific wound needs, such as antimicrobial agents, growth factors, or debridement agents.
6.1 Types of Dressings
Dressings vary widely, including hydrocolloid, foam, alginate, and antimicrobial options. Each type addresses specific wound needs, such as moisture control, infection prevention, or tissue debridement, promoting optimal healing environments.
6.2 Advanced Wound Care Products
Advanced wound care products include growth factors, bioengineered tissues, and negative pressure systems. These innovations promote tissue regeneration, manage exudate, and enhance healing in complex wounds. They are designed to address specific challenges, such as deep tissue deficits or chronic wound stagnation, offering tailored solutions for optimal patient outcomes.
6.3 When to Change Dressings
Dressings should be changed upon wound assessment, typically when they become saturated, loosened, or soiled. Signs like increased exudate, odor, or visible debris indicate a needed change. Frequency depends on wound type, depth, and healing progress, ensuring a clean environment for tissue repair. Proper timing balances infection prevention and avoids disrupting the healing process.

Pressure Ulcer Prevention
Pressure ulcers are preventable through risk assessment, regular repositioning, and proper support surfaces. Education and early intervention are key to reducing their incidence and improving patient outcomes.
7.1 Risk Factors for Pressure Ulcers
Risk factors for pressure ulcers include immobility, limited sensory perception, poor nutrition, and medical conditions like diabetes. Elderly patients, those with chronic illnesses, and individuals with compromised circulation are at higher risk. Identifying these factors early is crucial for implementing preventive strategies and reducing the likelihood of pressure ulcer development.
7.2 Strategies for Prevention
Effective prevention strategies include regular repositioning of immobile patients, use of pressure-redistributing support surfaces, and ensuring proper nutrition. Assessing risk factors and implementing tailored care plans are essential. Patient education on weight shifts and skin inspections can also reduce pressure ulcer incidence. Early intervention and multidisciplinary approaches further enhance preventive efforts.
7.3 Staging of Pressure Ulcers
Pressure ulcers are staged based on tissue damage severity, from Stage 1 (non-blanchable erythema) to Stage 4 (full-thickness skin loss). Accurate staging guides treatment and monitoring. Documentation is critical for tracking progression and response to interventions, ensuring optimal patient care and outcomes.

Certifying Organizations
Prominent certifying organizations like the National Alliance of Wound Care and Ostomy (NAWCO), Wound, Ostomy, and Continence Nursing Certification Board (WOCNCB), and American Board of Wound Management (ABWM) establish standards and credentials for wound care professionals, ensuring expertise and quality patient care.
8.1 National Alliance of Wound Care and Ostomy (NAWCO)
NAWCO is a non-profit organization dedicated to promoting excellence in wound care through certification. It offers credentials like the Wound Care Certified (WCC) for professionals, ensuring they meet high standards of knowledge and practice. NAWCO supports continuous education and professional growth, contributing to improved patient outcomes in wound management and ostomy care.
8.2 Wound, Ostomy, and Continence Nursing Certification Board (WOCNCB)
WOCNCB is a national certifying agency for nurses specializing in wound, ostomy, and continence care. It offers credentials like the Certified Wound, Ostomy, and Continence Nurse (CWOCN), ensuring expertise in managing complex conditions. WOCNCB certifications validate advanced knowledge and clinical skills, fostering high-quality patient care and professional advancement in specialized nursing fields.
8.3 American Board of Wound Management (ABWM)
ABWM is a certification body dedicated to elevating wound care standards. It offers credentials like Certified Wound Specialist (CWS) and Certified Wound Care Associate (CWCA). These certifications validate expertise in wound management, fostering advanced clinical skills and evidence-based practices. ABWM certification enhances professional credibility and contributes to improved patient care in wound healing and related specialties.
Exam Preparation Tips
Effective study habits, practice exams, and joining study groups are key to successful wound care certification preparation, ensuring comprehensive understanding and readiness for the exam.
9.1 Effective Study Habits
Developing effective study habits is critical for success in wound care certification. Create a structured study plan, set specific goals, and allocate time for consistent review. Utilize active learning techniques, such as highlighting key concepts and engaging with practice questions. Stay organized by prioritizing topics and reviewing challenging areas repeatedly. Regularly test your knowledge to identify gaps and refine your understanding of wound care principles and practices.
9.2 Practice Exams and Mock Tests
Practice exams and mock tests are essential tools for preparing for wound care certification. These resources simulate real exam conditions, helping candidates assess their readiness and identify knowledge gaps. Regularly taking practice tests improves time management, reduces anxiety, and enhances familiarity with question formats. Utilize detailed explanations to understand incorrect answers and reinforce learning, ensuring a comprehensive understanding of wound care principles and practices before the actual exam.
9.3 Joining Study Groups
Joining study groups enhances wound care certification preparation by fostering collaboration and shared learning. Group discussions allow participants to exchange insights, clarify doubts, and explore complex topics collectively. Active participation in study groups also builds confidence, provides diverse perspectives, and keeps candidates motivated throughout their exam preparation journey, ensuring a well-rounded understanding of wound care principles and practices. This collaborative approach strengthens both individual and group knowledge retention and application skills effectively.

The Role of Certification in Patient Care
Certification in wound care ensures healthcare professionals deliver evidence-based, high-quality patient care, promoting better outcomes and enhancing clinical expertise in wound management and treatment.
10.1 Improved Patient Outcomes
Certified wound care professionals utilize evidence-based practices, leading to faster healing, reduced complications, and enhanced patient comfort. Their expertise minimizes infection risks and promotes optimal tissue repair, resulting in improved quality of life for patients with acute or chronic wounds.
10.2 Enhanced Professional Competence
Certification in wound care elevates a professional’s expertise, ensuring they possess in-depth knowledge of wound assessment, treatment, and management. This specialized training fosters confidence and proficiency, enabling healthcare providers to deliver high-quality, standardized care, which is essential for achieving successful patient outcomes and advancing their careers in the field.
10.3 Career Advancement Opportunities
Obtaining wound care certification opens doors to advanced roles and specialized positions in healthcare. Certified professionals are highly sought after, leading to increased job opportunities, higher salaries, and recognition as experts in their field. This credential also positions individuals for leadership roles, fostering long-term career growth and the ability to contribute to cutting-edge advancements in wound care.

Comprehensive Study Guide Features
A comprehensive study guide offers detailed chapter reviews, practice questions, and evidence-based content, ensuring thorough preparation for the wound care certification exam.
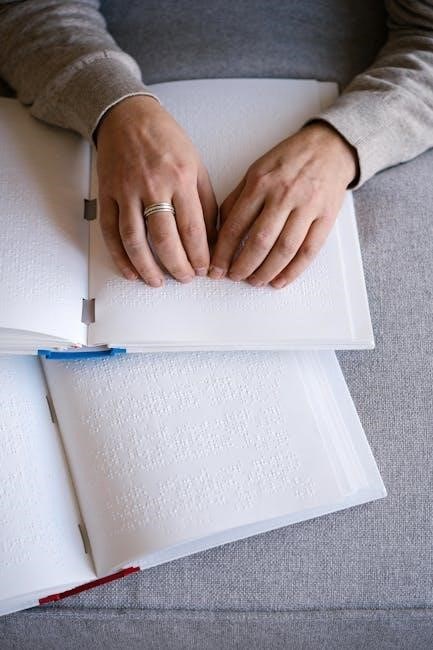
11.1 Detailed Chapter Reviews
Detailed chapter reviews in the study guide provide in-depth analysis of key topics, from wound assessment to healing physiology. Each chapter breaks down complex concepts, ensuring a thorough understanding of wound care principles and practices. Visual aids like diagrams and charts complement the text, making the content engaging and easier to retain. This structured approach helps candidates master essential knowledge for certification.
11.2 Practice Questions and Answers
The study guide includes an extensive bank of practice questions and answers, covering all key topics in wound care. These questions are designed to simulate real exam scenarios, helping candidates assess their knowledge and identify areas for improvement. Detailed explanations accompany each answer, providing clarity and reinforcing learning. Regular practice with these questions enhances exam readiness and confidence.
11.4 Evidence-Based Content
The study guide incorporates evidence-based content, ensuring that all information is supported by the latest clinical research and best practices. This approach guarantees that professionals receive accurate and up-to-date knowledge, enabling them to deliver effective wound care. The content is regularly updated to reflect advancements in the field, ensuring that certification candidates are well-prepared to meet current standards and patient needs effectively.